
Across Scotland, thousands of people provide unpaid care for family members, friends, or neighbours. They do this out of love – but it often comes at a cost to their own health.
Research shows that unpaid carers often experience poorer physical and mental health than people who do not provide care.
That’s why we’ve reopened our Supporting Change – Carers programme. The programme funds projects that help reduce health inequalities for unpaid carers by changing the systems around them – not just offering short-term fixes.
But what do we mean by systems change? Let’s break it down.
Why unpaid carers need better support
Research shows that unpaid carers often have poorer physical and mental health than people who do not provide care. Many experience loneliness, long-term pain or illness, and money worries caused by juggling work and caring.
These problems don’t happen by accident. They’re caused by the way our society, services, and attitudes are set up. To make things better, we need to look deeper than what we can see on the surface.
That’s why it’s vital to address these barriers and make changes to the systems around carers, to improve their health.
Thinking about systems change
To help us better understand systems change, we worked with Jennifer Wallace, a Senior Strategic Improvement Coach. She has lots of experience in public service innovation and policy development, with a focus on wellbeing and putting people at the centre of adult social care. Jennifer brings a deep understanding of how to make lasting changes in complex systems – helping us find ways to reduce health inequalities for unpaid carers.
Jennifer introduced us to and helped us use the iceberg model to explain systems change.
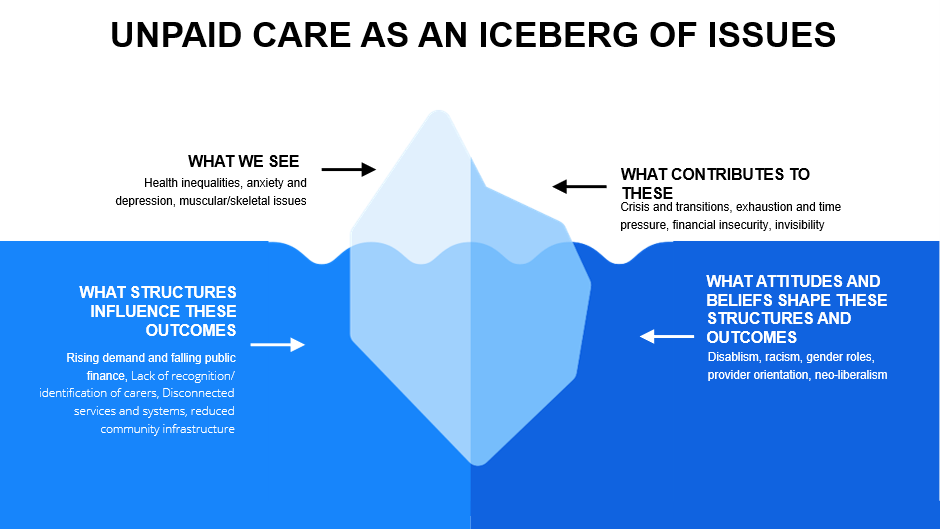
To explain what we mean by systems change, we use the iceberg model (pictured above). This model helps us to understand what drives health outcomes for unpaid carers and where change can make the biggest impact. The iceberg model (Figure 1) has four levels:
1: What we see when we look at unpaid carers and health outcomes?
2: What is happening to cause these outcomes?
3: What structures are influencing these patterns and outcomes?
4: What attitudes and beliefs shape these structures and outcomes?
Systems change means looking “beneath the waterline.” What we see (health outcomes) is supported by what we don’t see (structures and beliefs). For projects aiming at systems change, we want to fund projects that focus on influencing what is below the water –the structure, attitudes and beliefs that shape these structures.
Level 1: The Visible (What we see?)
These are the health problems unpaid carers often face, such as:
- More care needs due to an ageing population
- Different challenges at different ages (for example, young carers missing school or friends, older carers dealing with their own health issues)
- Trying to balance caring with inflexible jobs, which can lead to financial insecurity and poverty.
Level 2: The Patterns (What is happening?)
These are the things that happen again and again and lead to poor health outcomes.
- Cuts to public funding mean unpaid carers are doing more, with some communities unable to access the right support.
- Carers are often treated as an extension of the healthcare system instead of being recognised as equal partners with valuable lived experience.
Level 3: The Structures (Why is it happening?)
These are the rules and systems that make life harder for carers. Barriers that influence their health outcomes, include:
- Workplace norms prioritise continuous, full-time work, making it more difficult for those with care duties.
- Fragmented systems. For example, health, social care, and welfare services don’t always work well together leading to inconsistent support.
- Caring has slowly been seen as a private family issue, rather than something society should share responsibility for.
Level 4: The Mental Models (What beliefs shape this?)
These are the attitudes and beliefs that help to shape health inequalities, including:
- The belief that caring is “natural” for women.
- How race, sexuality, and disability compound the impact. For example, how women with ME (a chronic, often disabling condition sometimes also called chronic fatigue syndrome – are overrepresented in care but under-supported).
- How care is excluded from economic indicators like GDP, so it’s easy for decision-makers to overlook when planning services and support.

What we want to fund
Though Supporting Change Carers, we want to fund projects that don’t just help carers cope – but help change the system itself. This means funding community-led initiatives that tackle the root causes of challenges, create long-term health benefits for unpaid carers, and reduce the inequalities they face.
Ideas we will consider include those that:
- Challenge unfair structures
- Shift attitudes and beliefs
- Create long-term improvements to carers’ health
- Reduce the inequalities unpaid carers face
Find out more
You can learn more about the Supporting Change Carers programme on our website. You can also sign up for one of our upcoming information sessions for more detail.